The fight against COVID-19 has infiltrated every aspect of our lives, from disrupting work to shuttering schools and sidelining almost every event of 2020.
By Derek Herscovici ’14
The fight against COVID-19 has infiltrated every aspect of our lives, from disrupting work to shuttering schools and sidelining almost every event of 2020. But while many of us watch from home, our nation’s medical professionals are on the front lines of this deadly disease, fighting for the survival of their patients while risking the health of themselves and their families. These are the experiences of Auburn alumni in their own words, edited for clarity and length.

MSN, RN, CRNP — Madison Hospital Emergency Department
Madison, Ala.
How has your line of work been affected by COVID-19?
I had a baby in February and was out on maternity leave when COVID was first ramping up. I was scheduled to go back to work May 3 but because the ER census was down due to fears of COVID I was furloughed until about May 25. Since then our volumes have continued to increase. COVID had been fairly well contained in north Alabama until the last few weeks and now we are having higher patient volumes as more people want to get tested and treated for COVID. I was very apprehensive about going back to work. I still change into hospital issued scrubs at work, undress outside when I get home, and always shower before interacting with my children. I’m so nervous I will infect my 4 month old.
Can you describe the current situation in your workplace?
For the last week it’s been busy and our COVID section has been full in the ER. So far none of the nurses or physicians in our department have tested positive (as far as I know) and we have plenty of PPE. I am also working at our fever and flu clinic occasionally, and I saw 70 patients in one 8 hour day last week, which is more than I’ve ever done.
What have the last few weeks been like, in your own words?
To sum it up in one word, troubling. It is upsetting to see masks politicized when it is a simple and easy solution to reducing spread. Recently leaders in our area have suggested our limiting factors wouldn’t be beds or ventilators when things get bad, but that it might be medical personnel. I am increasingly nervous not only for myself on the front line but for my family.
How has your home or personal life been affected by the pandemic?
Several family members have not gotten to meet my new baby. I didn’t get to spend father’s day with my dad. I think working in such a high risk area makes my extended family and friends understandably nervous to spend time with me. I really miss spending time with them.
How did Auburn prepare you for your current role?
When I was in nursing school at Auburn it felt rigorous and strict, but boy was that a blessing in disguise. Auburn’s Nursing program was excellent and prepared me for a career that also turned out to be quite rigorous. Not only was I thoroughly prepared knowledge wise to take on my role as a nurse, I knew how to work hard.
How do you stay positive during these difficult times?
My husband and kids really keep me going. I have a two year old son who always keeps me laughing and sweet new baby to cuddle. Home is a nice retreat when the world seems so crazy. When I can steal some time to exercise it always makes me feel better, especially when I start to feel overwhelmed/anxious.
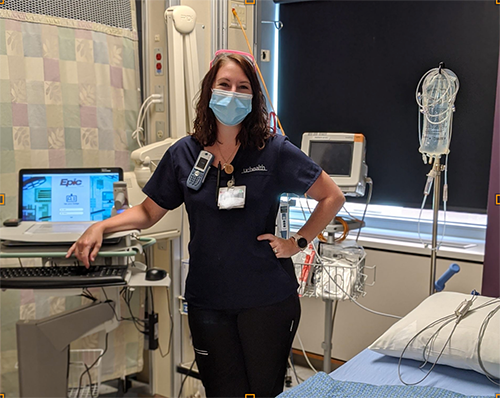
Registered Nurse — UCHealth Cardiac Cath Lab
Aurora, Colo.
How has your line of work been affected by COVID-19?
My unit preps/performs/recovers all cardiac procedures. We have had our fair share of Covid positive patients come through the unit. Our PPE guidelines and restrictions have gotten much more detailed and complicated now that we are needing to protect ourselves and other patients from Covid. We are required to wear a regular mask for the duration of our shift and have to switch into N95 masks while scrubbed into procedures. We are also using face shields, goggles, and gowns for covid positive or rule-out cases. The majority of our patients are outpatient and come in the day of their procedure. These patients are now required to get a covid test done within a week of their appt time. All inpatient cases are being tested too, time allowing. Our PPE guidelines remain the same regardless of test result, however. In terms of how we’ve been affected, i would say we’ve had to slow down our process greatly because of all the extra precautions we are needing to take, and this has caused us to be working much longer hours now that patients are recovering later into the evening and then being discharged home.
Can you describe the current situation in your workplace?
During the peak of Covid-19 in Colorado, my unit had cancelled all elective/non-emergent cases so as to decrease exposure to both staff and patients. That being said, we were still doing emergent pacemakers, heart catheterizations, cardioversions, etc; many of which were Covid positive patients. Now that out peak has passed, we have begun rescheduling these cancelled procedures. We are just as busy as before but there are more restrictions in place now. Patients require testing prior to their appt time, only one visitor/support person can come to the hospital with them any must remain in the waiting room for the duration of the procedure and recovery time. We have also had to make changes to the way we scrub our procedures. Because of the amount of PPE required during these cases, we have to have extra staff available to help supply the scrub team with supplies and medications. While we are still able to do our jobs effectively, our process has slowed down, especially when it comes to cleaning rooms in between patients, involving ancillary staff in care, and providing discharge instructions to family members or visitors.
What have the last few weeks been like, in your own words?
The Covid-19 pandemic reached Colorado in early March; our Stay At Home order was implemented on March 12 and was only lifted at the beginning of June. It does seem surreal sometimes, driving to work, when you’re the only car on the road. Entering the hospital itself has it own challenges. We must take our temperature and record it in an app 30 minutes prior to our shift start time, show the check at the door, and have a mask on in order to get to our units. For quite a while, we had been sending used masks down to the sterile processing department (SPD) to be reprocessed and placed back into circulation. Working as a nurse during the Covid-19 pandemic has been very trying, to say the least. One of the more challenging aspects, to me, was seeing how serious this virus is first hand, seeing the crowded ICUs and exhausted staff…and still seeing people in public not wearing masks or taking precautions. It became easier to just stay at home and not be in public at all so that I wouldn’t get frustrated or saddened by the people not taking it seriously. On several occasions, we even had family members in the hospital refusing to wear a mask and were eventually asked to leave by upper management. It has been very tough to spread awareness without spreading fear.
How has your home or personal life been affected by the pandemic?
My husband is also a nurse (cardiac) and we do not have anyone else in our home. While that does reduce some risk because we have an equal chance for exposure, we still took drastic precautions when returning home. We made a rule that no dirty scrubs entered the house and all work shoes remained at the hospital or in the garage. We isolated ourselves from friends and family through May and now only visit with people outdoors. I would say that, other than being stuck at home, our home life hasn’t been affected too much, just because my husband and I are in the same line of work. It does, however, make you rethink whether your sore throat is allergies or something worse….
How did Auburn prepare you for your current role?
During my final semester of nursing school, I was assigned to do my final practicum/preceptorship on a cardiac unit in Atlanta, where I lived at the time. While I had no interest in cardiology at that time, it has grown to be quite a passion for me. I have been a nurse for 6 years and have spent my entire career in cardiology, working on the cardiac inpatient unit, outpatient cardiology office, and now cardiac procedural. I am forever grateful for Auburn for placing me on that cardiac unit to train because it has become a part of me; I love the heart.
How do you stay positive during these difficult times?
Communication is key. Even during quarantine, I made it a point to speak with my friends and family often. Most of my family works in healthcare too so they are familiar with what I’ve been doing. The important part is remembering to talk about what you’re feeling. There’s no room for heroes when trying to save lives. When work gets too heavy and you feel like crying or just feel too exhausted…that’s okay. You have to remember to take care of yourself so you’re at your best when others need you.
We Were CAPERS
From the 1960s to the 1980s, Auburn’s all-female military auxiliary instilled discipline and service, paving the way for future equality in the nation’s armed forces and preparing them for a lifetime of success.
The Antonio Network
Former Auburn football star Antonio Coleman ’08 returned to his old high school as head coach to turn the football program around. Through a unique group of local alumni, the team has started winning off the field, too.
Sharks, Sea Lions and Spreadsheets
Kristen Rosenberger ’10 keeps the National Aquarium swimming in the right direction.
Six Degrees of Separation
After Senior Lecturer Joseph Fetsch ’14 earned his first Auburn degree a decade ago, he kept going. Now he’s working on his sixth.
Auburn Tradition: The History of Hey Day
Get to know the Auburn Family with this one-of-a-kind campus tradition!
From Luck to Success: Lt. Col. Michael “Lucky” LaChance ’84
Doctors said he was dead, but it was just the beginning.
We Were CAPERS
From the 1960s to the 1980s, Auburn’s all-female military auxiliary instilled discipline and service, paving the way for future equality in the nation’s armed forces and preparing them for a lifetime of success.
Remember “The Old Breed”
The Bible of Eugene B. Sledge ’49, foundation of his classic World War II memoir “With the Old Breed,” was formally added to the Library of Congress this summer. His son Henry Sledge ’88 is still discovering how his family was shaped by the trauma of war.
Orange and Blue Angel
New Blue Angel Lilly Montana keeps her team flying in formation.







